A root canal is a dental treatment to preserve a tooth with an infected or inflamed pulp due to a deep cavity or trauma.
Despite its bad name, the dreaded root canal is not supposed to be painful.
However, root canals carry some risks. There is also much controversy about this treatment, which has caused concern and even fear.
This article will discuss what a root canal is, how to know if it’s the right treatment for you, its safety, what to expect, and more.
What is a root canal?
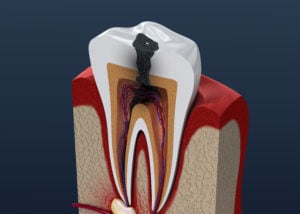
Root canal therapy is a type of dental procedure to preserve a tooth after the tooth’s pulp has become infected or inflamed. This is usually due to a deep cavity or trauma to the teeth or face.
The pulp is the tooth’s inner soft tissue containing connective tissue, nerves, and blood vessels.
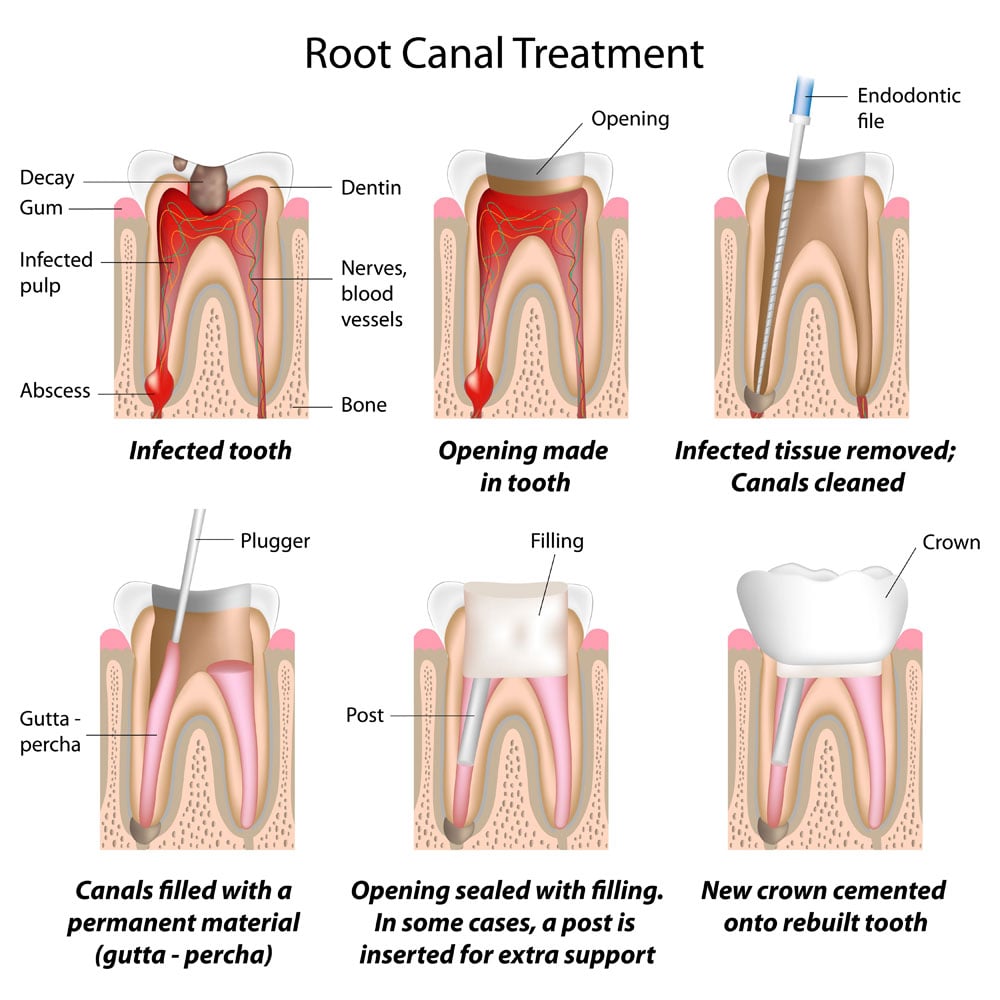
In a root canal procedure, your dentist or endodontist will clean out the infected tissue from the pulp chamber, then disinfect, fill, and seal the tooth. A crown will be placed over the tooth to preventing chipping or fracture.
A root canal procedure allows your dentist to preserve (not save) an infected tooth by removing infected tissue and sealing it.
Root canal procedures may also be referred to as:
- Endodontic treatment
- Root canal therapy
- Root canal treatment
- Root canal

Root canals are used to treat a condition called irreversible pulpitis.
Pulpitis (inflammation of the pulp) can be reversible or irreversible.
Irreversible pulpitis results when the nerve tissue dies as the pulp’s infection spreads.
Once a tooth gets to this point, the tooth cannot be saved as a vital (living) tooth.
But a root canal can preserve the tooth so that you don’t have to lose it.
Preserving your tooth benefits your oral health because it keeps your bite and teeth’ alignment stable. If your tooth is extracted and not replaced by an implant, your teeth may shift and cause alignment problems.
Tooth fracture is extremely common after a root canal. The tooth has been cleaned out, leaving the outer shell of the tooth dry, brittle, and prone to breakage.
A dental crown is usually required afterward to protect and strengthen the tooth.
A crown is like a cap (formed to look like a natural tooth) that covers the tooth to protect and preserve the tooth’s structural integrity.
How do I know if I need a root canal?
What conditions require root canal treatment?
Irreversible pulpitis (infection and inflammation of pulp) due to a deep cavity or trauma requires a root canal.
It’s impossible to heal or reverse irreversible pulpitis.
You may be able to catch pulpitis before it becomes irreversible. You want to catch and treat a cavity before it gets too big. This means following good oral hygiene and dental care, not skipping your dental checkups, and seeing your dentist as soon as you notice a toothache.
Signs you need a root canal may include:
- Toothache: Pulipitis will cause pain that is constant or intermittent. It may get worse when you chew or bite down. A sign of pulpitis is lingering pain from hot or cold stimuli that remain for seconds, minutes, or even hours. A sign of a tooth abscess is pain when you lay down or stand up (aka positional pain). Spontaneous pain that occurs without warning may indicate an inflamed pulp. Referred tooth pain that manifests in other areas of your head, such as other teeth, your face, or jaw, is also a sign of pulpitis.
- Deep cavity: a deep cavity can cause pain and the signs mentioned above. An x-ray will reveal a large cavity that has reached the pulp.
- Color change: The dying tooth may turn a grayish color over time. The gums can also darken around the tooth.
- Cracked tooth: If there is a fracture running down into your tooth root, it is unrestorable and requires either a root canal or an extraction.
- Tooth abscess: A tooth abscess (aka periapical abscess) is an infected, pus-filled area under the tooth root caused by bacteria and infection speaking down into the root
- Bump on the gum (fistula): A small white, yellow, or pimple-like fistula may appear on the gum as the body tries to “vent” the toxins from the infection.
- Swollen gums: The gums can become inflamed as the infection from the tooth spreads.
- Loose tooth: Your tooth can become mobile as the infection spreads from the tooth to the gums, ligaments, and bone.
Root canal diagnosis
Diagnosing a root canal requires x-rays, an oral exam, and diagnostic tests. This will allow your dentist to determine if the tooth is vital or dying, the severity of the infection, and what type of treatment is required.
What if i have no pain?
Whether or not you have pain, if your dentist diagnoses irreversible pulpitis, you will need a root canal.
Sometimes, if your tooth nerve dies, this may temporarily relieve the pain.
If the infection is big, your dentist may put on you antibiotics to reduce the infection before starting treatment. This will help relieve some of the pain, and your procedure will be more comfortable.
Untreated irreversible pulpitis can lead to serious harm to your health, so don’t hold off.
Your dentist must be positive that you have irreversible pulpitis before doing a root canal unnecessarily. In some cases, a root canal is not always necessary.
For example, if the pulpitis is reversible, a filling or a crown may suffice.

And in other cases, extraction and implant is a better long-term solution. For example, a tooth with extensive damage and decay with little tooth structure remaining has a poor prognosis (it wouldn’t last very long after the root canal) so extracting it and placing an implant is more cost-effective in the long run.
If your case is complex and requires specialized treatment, your dentist may refer you to an endodontist (root canal specialist).
Root canal procedure
How long does a root canal take?
A root canal procedures usually take 1 or 2 visits. Each visit will be around 60-90 minutes, depending on how complex the case is.
Before the procedure
Before beginning, your dentist will take an x-ray of the tooth.
If you are immune-compromised, have an abscess, or have a big infection, your dentist may prescribe antibiotics before the procedure.
During the procedure
Here is the step-by-step procedure of a Root Canal:
- X-rays and exam: Your dentist will do an exam and take additional x-rays. Multiple x-rays will be taken throughout the procedure to verify that the instruments are in the correct location for removing the infected tissue.
- Anesthesia: You will receive full local anesthesia to numb the tooth and surrounding area. If you’re nervous, you can request nitrous oxide (aka laughing gas), oral or IV sedation.
- Isolation: A covering (dental/rubber dam) will be placed over your mouth to protect you and prevent bacteria from getting into the tooth.
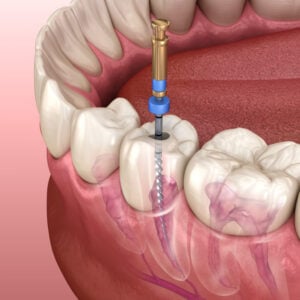
- Opening: An opening will be made at the top of your tooth to open up the pulp chamber.
- Cleaning and shaping: Your dentist will carefully remove the infected pulp tissue using fine files and drills. And the inside of the tooth will be thoroughly cleaned and shaped.
- Irrigation: Your dentist will irrigate the pulp chamber with water and antibacterial medicament to eliminate the bacteria and infection.
- Fill and Seal: After the pulp chambers are prepped and dried, your dentist will fill and seal the tooth. The tooth is filled with a biocompatible material called gutta-percha. Then a filling will be placed.
- Crown (if required): Once the root canal is completed, you’re ready for the crown.
Note: not every case requires a crown after a root canal.
Do root canals hurt?
Root canals should not be painful during the procedure as long as you are properly anesthetized. You may have some soreness and mild pain as you recover, depending on how big the infection was.
You can still drive home afterward because only local anesthesia is used. But if you opt for oral or IV sedation, you will need someone to drive you home afterward.
Root canal procedure: before and after
As your dentist gets inside the tooth during the procedure, new information may present itself that may change the root canal’s success.
If the new information lowers the chance of success than originally expected, your dentist will inform you.
From there, you can both decide if you want to stop or proceed.
Situations to stop a root canal include:
- Fracture: Once the tooth is opened, your dentist may see a fracture that wasn’t visible in the x-ray. In this case, an extraction with a dental implant is a better option.
- Calcified root canal: If the root canal is calcified, your dentist won’t be able to clean and shape it properly. This may require endodontic surgery.
- Separated instrument: A file or instrument tip may break off inside the tooth.
- Curved root: A tooth with a curved root is difficult to treat because of twists and turns making it difficult to treat successfully.
If the conditions aren’t ideal, your dentist will not proceed with the root canal. He or she may recommend a better treatment option for better long-term success.

Getting a crown
After the root canal therapy is complete, you will need to get a crown or filling a soon as possible.
If you wait too long (more than 4 weeks), you risk losing your investment in the root canal if the tooth fractures or gets reinfected.
Do you always have to get a crown after a root canal?
Most teeth require a crown after a root canal. However, front teeth (incisors and canines) don’t always require a crown, and your dentist will place only a filling.
Why get a crown?
Crowns have the following benefits for root canal treated teeth:
- Higher success rate: A root canal will last much longer if the tooth is covered with a crown. Otherwise, the chance of fracture or reinfection significantly increases.
- Aesthetics: A crown can be made to match the other teeth and hide any discoloration.
Antibiotics & root canal therapy
Antibiotics are often prescribed in addition to root canals to reduce the risk of pain and systemic infection. However, not every root canal requires additional antibiotic treatment.
It’s also important to consider the risk of antibiotic resistance from unnecessary and frequent use of antibiotics.
Studies show that antibiotics are truly needed in the following circumstances:
- tooth abscess in an immune-compromised patient
- systemic infection caused by a tooth abscess
- rapid onset of infection with apparent symptoms within 24 hours
- replantation of an avulsed tooth (a tooth that was knocked out)
- extensive trauma to the mouth tissues
How long can I go before getting a root canal?
You never want to wait to get a root canal (or alternative treatment) once your dentist diagnoses irreversible pulpitis.
The longer you wait, the worse the infection and pain will get.
And the longer the infection goes untreated, the higher the chances of complications, which can be life-threatening. So please don’t wait!
Root canal recovery
It’s not uncommon to experience some discomfort for a few days after a root canal. Remember not to smoke for at least a week after a root canal. And avoid chewing hard, sharp, hot (in temperature) or spicy foods and beverages for a couple of days. Avoid drinking alcohol for 1-2 days. And don’t bite or chew on the treated tooth until a crown is placed. Continue good oral hygiene care as normal.
Can you drive after a root canal? Root canals usually only require local anesthetic, so you should be able to drive immediately after a root canal procedure unless you opted for sedation.
Make sure to go to your root canal follow-up visit (6 months later) and your regular dental check-ups so your dentist can continue to monitor your root-canal-treated tooth.
Pain after a root canal
You may experience some pain within the first day or so after a root canal. You might also have soreness from keeping your mouth open for a long time. If you’d like, you can use over-the-counter pain medications to relieve any pain. But these symptoms should resolve in 1-2 days.

If you have TMJ disorder, your jaw may be sore for several weeks.
The gums around the treated tooth may also be sore and inflamed for a couple of days due to the root canal treatment. But this should resolve in about a week or two.
I recommend warm salt water rinses 3 times a day which helps soothe the gums, promote healing, and reduce inflammation.
If you experience persistent pain, this could be caused by:
- a severe infection before your root canal
- existing chronic pain
Sometimes, a filling can be too high and cause pain upon biting. Your dentist can easily adjust this for you, and symptoms should go away in 1-2 weeks.
If you experience severe pain weeks or months after your root canal, the root canal may have failed. Make sure to see your dentist as soon as possible.
Root canal cost
A root canal may cost you anywhere from $600-$2,000, depending on the tooth’s location and condition. Root canal specialists (endodontists) usually charge around 50% more for a root canal.
With the crown’s cost added on, the total cost can be anywhere from $1200-$3500, depending on the material used for the crown.
How much does a root canal cost with insurance?
Most dental insurances will cover root canals, but the rate of coverage varies by plan. Also, your coverage will usually apply only once you’ve met your deductible.
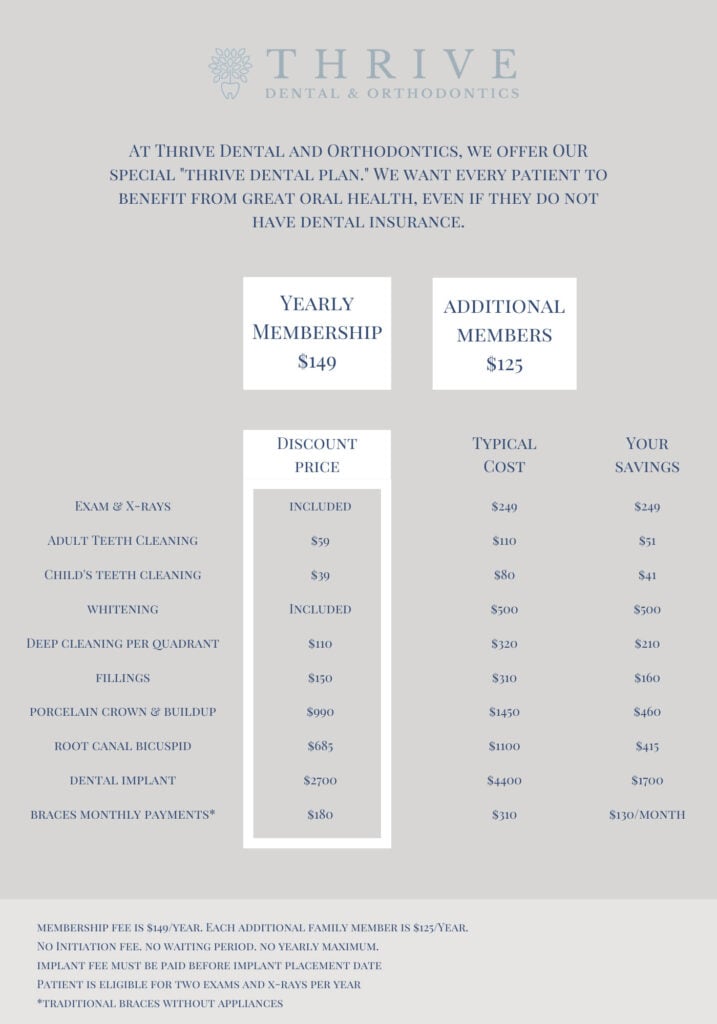
Don’t have dental insurance? We’ve got you, friend.
Take advantage of our Thrive Dental Discount Plan, where we offer significant discounts on our dental services for an annual fee of only $149.
We believe everyone deserves excellent dental care, and that it should be affordable.
Are root canals worth it?
Yes, root canals are worth the time and money put into them. They have a high success rate (when a crown is placed) and cost much less than an extraction with a dental implant or dental bridge.
However, if you have other medical or dental conditions, this can decrease your root canal’s long-term prognosis.
Risks of root canal therapy
There are some possible complications of root canal treatment to be aware of.
There’s the risk of reinfection after a poorly done root canal. If the root canal was not adequately cleaned, filled, and sealed, or if there is a broken instrument present, the chances for reinfection increase.
If the tooth or root were accidentally perforated during root canal treatment, the tooth would most likely need extraction.
You may also experience pain if the root canal was overfilled or any sinus drainage from a large abscess allowing the disinfecting solution to get into the sinus. These issues usually resolve on their own in a couple of weeks. However, if you experience sharp and/or sudden pain, see your dentist right away.
Therefore, it’s crucial that your dentist or endodontist does a good job on your root canal to avoid future problems.
Prognosis
Root canals have a high success rate if a crown is placed on the treated tooth. However, if the tooth was necrotic (dead), had a large infection, was fractured, or if you have periodontal disease, untreated tooth decay, or new bacterial infection, your root canal’s success diminishes.
How long does a root canal last?
A root can last about 10 years or more (even a lifetime) if done correctly and cared for properly.
Are root canals safe?
Root canals have been used for ages, and they are safe for most people. To ensure your root canal is holding up, it is recommended to get a CBCT (cone beam CT) every 3-5 years to check for failure.
Recently, there has been a lot of controversy over the safety of root canals. While the ADA (Amerian Dental Association) confirms that root canals are safe and provide many benefits, other schools of thought argue that we should avoid root canals at all costs.
The recent Root Cause documentary (which is now banned) claimed that root canals are extremely dangerous and the “root cause” of many systematic diseases.
However, there is no scientific evidence that supports these claims.
But if you happen to be at risk for root canal failure (such as immuno-compromised patients), it might benefit you to seek an alternative treatment.
Summary
In conclusion, a root canal is used to treat irreversible pulpitis, which cannot be healed or reversed.
During a root canal, your dentist will disinfect, shape, and seal the inside of the tooth. Then a filling will be placed, and a crown will usually be placed.
The cost of a root canal ranges from $600-$2,000, depending on your tooth’s location and condition. The cost will be around 50% more if you go to an endodontist (root canal specialist). Your insurance usually provides some coverage for root canal treatment and varies per insurance provider.
It’s never a good idea to wait on getting your root canal, as this could eventually lead to complications that can be life-threatening.
If you have a toothache or any symptoms of pain or inflammation, see your dentist right away.
At Thrive, we provide same-day emergency visits so we can get you the help you need as soon as possible.
Call (972) 371-0616 or Book Online now.
by: Dr. Christine Coughlin DDS
Learn More: